Newborns with vitamin D deficiency have an increased risk of schizophrenia later in life, a team of Australian and Danish researchers has reported.
The discovery could help prevent some cases of the disease by treating vitamin D deficiency during the earliest stages of life.
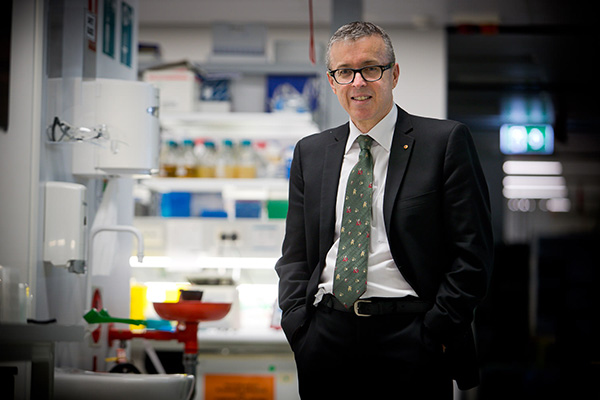
The study, led by Professor John McGrath from The University of Queensland and Aarhus University in Denmark, found newborns with vitamin D deficiency had a 44 per cent increased risk of being diagnosed with schizophrenia as adults compared to those with normal vitamin D levels.
“Schizophrenia is a group of poorly understood brain disorders characterised by symptoms such as hallucinations, delusions and cognitive impairment,” he said.
“As the developing foetus is totally reliant on the mother’s vitamin D stores, our findings suggest that ensuring pregnant women have adequate levels of vitamin D may result in the prevention of some schizophrenia cases, in a manner comparable to the role folate supplementation has played in the prevention of spina bifida.”
Professor McGrath, of UQ’s Queensland Brain Institute, said the study, which was based on 2602 individuals, confirmed a previous study he led that also found an association between neonatal vitamin D deficiency and an increased risk of schizophrenia.
The team made the discovery by analysing vitamin D concentration in blood samples taken from Danish newborns between 1981 and 2000 who went on to develop schizophrenia as young adults.
The researchers compared the samples to those of people matched by sex and date of birth who had not developed schizophrenia.
Professor McGrath said schizophrenia is associated with many different risk factors, both genetic and environmental, but the research suggested that neonatal vitamin D deficiency could possibly account for about eight per cent of schizophrenia cases in Denmark.
“Much of the attention in schizophrenia research has been focused on modifiable factors early in life with the goal of reducing the burden of this disease,” he said.
 “Previous research identified an increased risk of schizophrenia associated with being born in winter or spring and living in a high-latitude country, such as Denmark.
“Previous research identified an increased risk of schizophrenia associated with being born in winter or spring and living in a high-latitude country, such as Denmark.
“We hypothesised that low vitamin D levels in pregnant women due to a lack of sun exposure during winter months might underlie this risk, and investigated the association between vitamin D deficiency and risk of schizophrenia.”
Professor McGrath said that although Australia had more bright sunshine compared to Denmark, vitamin D deficiency could still be found in pregnant women in Australia because of our lifestyle and sun-safe behaviour.
Professor McGrath, who holds a prestigious Niels Bohr Professorship at Aarhus University, also led a 2016 Dutch study that found a link between prenatal vitamin D deficiency and increased risk of childhood autism traits.
“The next step is to conduct randomised clinical trials of vitamin D supplements in pregnant women who are vitamin D deficient, in order to examine the impact on child brain development and risk of neurodevelopmental disorders such as autism and schizophrenia.”
The research was published in Scientific Reports (DOI: 10.1038/s41598-018-35418-z) and was supported by organisations including Australia’s National Health and Medical Research Centre, the Danish National Research Foundation, The University of Queensland, the Clem Jones Centre for Ageing Dementia Research, the Lundbeck Foundation, and the European Research Council.
Media contact: QBI Communications, communications@qbi.uq.edu.au, +61 405 661 856.
Video and audio grabs are available from:
https://www.dropbox.com/sh/v4smkfir2qcsq7r/AAAjEuYrZ5dW2E1sd1c546sta?dl=0.
.jpg)