Dangerous antibiotic-resistant bacteria could soon be targeted with a drug initially developed to treat Alzheimer’s disease.
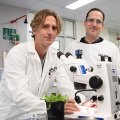
University of Queensland-led research investigated the antibacterial properties of metal transport drug, PBT2.
Professor Mark Walker from UQ’s School of Chemistry and Molecular Biosciences said while the drug did not make it to market for Alzheimer’s and Huntington’s disease, the results suggest it may still have great use.
“This particular drug progressed to phase one and two human clinical trials for Alzheimer’s and Huntington’s, and was shown to be well tolerated by human subjects,” he said.
“PBT2 is designed to disrupt the interaction between metals and human cells, which was thought would reduce heavy metal levels in the brain.
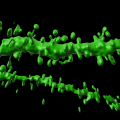
“With this in mind, and knowing that disrupting metal content can induce toxicity in bacteria, we examined the effects of PBT2 against a wide range of antibiotic-resistant bacteria.”
The results indicated that the drug had the capacity to fight infectious diseases by breaking antibiotic-resistance in bacteria.
“Repurposing PBT2 as an ‘antibiotic breaker’ represents a new strategy in the fight against antibiotic-resistant bacteria,” Professor Walker said.
“We may be able to reverse it in such a way that ineffective antibiotics become effective again in treating infectious diseases.”
Professor Mark von Itzstein from Griffith University said it was exciting news, given that antibiotic resistance is one of the greatest threats to global public health.
“Over the past 30 years, many species of bacteria have acquired resistance to a wide range of antibiotics,” he said.
“This has rendered current antibiotic treatment therapies ineffective and led to increasing numbers of deaths due to infectious disease agents in Australia.
“If new solutions aren’t developed, it’s estimated that by 2050, antimicrobial-resistant bacteria will account for more than 10 million deaths per year.
“We’ve found one more weapon in our arsenal to help save millions of lives.”
The research was led by the Australian Infectious Diseases Research Centre, UQ, and the Institute for Glycomics, Griffith University, and has been published in mBio (DOI: 10.1128/mBio.02391-18).
Media: Professor Mark Walker, mark.walker@uq.edu.au, +61 3346 1623; Dominic Jarvis, dominic.jarvis@uq.edu.au, +61 413 334 924.
.jpg)