A new triple-combination drug treatment being trialled at the Mater Hospital in Brisbane could increase the life expectancy of patients with cystic fibrosis.
Mater Research Institute-University of Queensland (MRI-UQ) researcher Dr Lucy Burr said seven patients were enrolled in Phase 2 of the clinical trial, which aimed to treat the underlying cause of cystic fibrosis.
“A new drug, known as VX-445, in combination with two existing treatments, has demonstrated lung function improvement of around 10 per cent – which is really significant for cystic fibrosis patients,” Dr Burr said.
“Patients in our trial had significant increases in their lung function that they hadn’t been able to achieve previously.”
Dr Burr said the early phase study showed some exciting progress.
“In cystic fibrosis, most patients will die from lung disease, so improving or maintaining their lung function is the mainstay of treatment.”
In Australia, a baby is born every four days with cystic fibrosis.
There is currently no cure for the genetic disorder which primarily affects the lungs and digestive system, reducing life expectancy to 37.
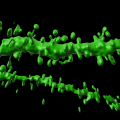
Dr Burr said that in cystic fibrosis, a protein called CFTR did not do its job of transporting salt and water in and out of cells.
“This affects the pancreas, liver, lungs, sinuses… everything,” Dr Burr said.
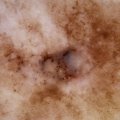
“A lot of our therapies are directed at treating the consequences of CFTR dysfunction: decreased lung function, bowel function, pancreatic problems and really thick, sticky, dehydrated mucus.
“There are two drugs on the market in Australia which target the CTFR protein to make it work better in patients with specific gene mutations – giving access to treatment for about 50 per cent of the cystic fibrosis population.
“This triple combination has the potential to treat 90 per cent of patients.”
Dr Burr said the trial used the triple-combination therapy, to target the CFTR protein in patients with a ‘F508del’ gene mutation.
“Two of the drugs help the protein move through the cell, and one of the drugs helps the protein channel open,” she said.
“Adding the extra drug seemed be the key to making the dual combination work much better.
“The drug improved the protein function, which we measured through sweat chloride in patients.
“It also significantly improved their lung function and quality of life – and that was only over a four week period.”
Dr Burr said the development of drugs that target the CFTR was an exciting step forward for cystic fibrosis care.
“When you’re targeting the actual problem, there’s great potential for these medications to change, and lengthen, the lives of patients with the illness.”
Mater is currently participating in Phase 3 of the clinical trial.
The study is published in the New England Journal of Medicine (DOI 10.1056/NEJMoa1807120).
Media: UQ Faculty of Medicine, med.media@uq.edu.au, +61 7 3365 5133, +61 (0)436 368 746.
.jpg)