-1.jpg?itok=JOES18M7)
Cone snail venom has given University of Queensland researchers a lead on the possible detection and treatment of some cancers and addictions.
UQ School of Biomedical Sciences’ Dr Richard Clark said cone snails produced a venom that immobilised prey including worms, other snails and fish.
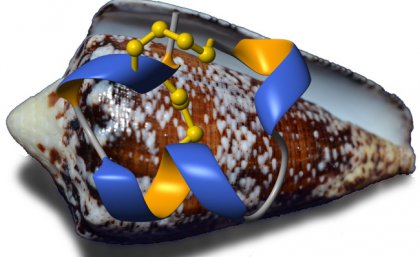
“This venom contains hundreds of different toxins that are highly potent and target specific receptors in their prey,” he said.
“The power and selectivity of these toxins make them both valuable drug leads and excellent molecular tools for understanding the human body’s processes.
Dr Clark said some of the toxins targeted the nicotinic acetylcholine receptor (nAChR) family.
“These receptors in the nervous system play diverse roles and have been implicated in a range of diseases including Alzheimer’s disease, schizophrenia, tobacco addiction and lung cancer.”
Dr Clark said the activation of one type of nAChR receptor, alpha3beta4, had been associated with lung cancer and nicotine addiction.
“However, understanding of this process has been limited and it has been shown in previous studies that a specific toxin from the cone snail venom inactivated the alpha3beta4 nAChR but also inactivated other types of nAChR,” he said.
“Our study focused on a specific toxin and we investigated its structure and how it worked to see if we could engineer a molecule that would only target the receptor associated with cancers and addictions.
“We were able to do this and it can now be used as a tool for studying these diseases.
“It might also be a potential drug lead once more is known about the role of the receptor in these conditions."
The study, published in The Journal of Biological Chemistry, was done in collaboration with Royal Melbourne Institute of Technology’s Professor David Adams and Dr Frank Mari from the Florida Atlantic University in the USA.
The research was supported by Australian Research Council funding.
Media: Dr Richard Clark, +61 7 3365 1527, +61 (0)439 667 604, Richard.clark@uq.edu.au or Bernadette Condren, Faculty of Medicine and Biomedical Sciences media manager, +61 7 3346 5309, b.condren@uq.edu.au.
.jpg)