Septic shock is a condition that kills 3.5 times more people each year than the national road toll – yet we rarely hear about it in the news.
Septic shock is a life-threatening complication of sepsis (infection that has reached the bloodstream) and is a major cause of death in patients admitted to Intensive Care Units worldwide. Septic shock causes vital organs to shut down, and once diagnosed, life expectancy is less than 90 days for one in three patients.
Septic shock can originate from a bacterial, fungal or viral infection and is notoriously difficult to treat. One theory is that the infection (sepsis) triggers a complex response by the body (the inflammatory response) that causes a decrease in blood pressure preventing oxygen and nutrients from reaching organs and so starving them. What compounds the problem is that medication that works for one person may not necessarily work for another. One size definitely does not fit all.
This is where Professor David Evans and his team at the UQ Diamantina Institute come in. Collaborating with scientists from The George Institute for Global Health and other institutions, they are producing a library of genomic material from 25 different sites in Australia and New Zealand that can be used to test which treatments may work for particular people and which may not.
“What we are doing is collecting hundreds of blood samples from critically ill patients diagnosed with septic shock, and then analysing which genetic markers sufferers may have in common when responding to treatment or becoming worse,” says Professor Evans.
“In other words, does a person’s genetic make-up cause them to be more susceptible to general infections? Or influence how sick they get actually get? Or whether they respond to conventional medicine?
“That’s what we want to find out.”
Septic shock affects 15,000 people per year in Australia, plus millions worldwide, and so any treatment improvements will make a significant difference to recovery and quality of life. With a cost of around $42,000 per episode, they will make a significant impact on health expenditure too.
“At present, there is considerable uncertainty as to what the best treatment is for patients suffering sepsis and septic shock,” says Professor Evans.
Over the past two decades, researchers have trialled more than 70 possible alternatives, but results have been disappointing. The most promising adjunctive therapy of late, activated protein C, was withdrawn from the market in 2011 after a trial failed to confirm its efficacy.
And there is no consensus about the use of corticosteroid therapy, as conflicting results were produced in two of the most recent trials.
Professor Evans and his team hope that if particular sectors of the population can be defined as suitable candidates for steroid treatment before receiving the drug, fewer people will die. Applying a more personalised approach to treatment may be the way forward.
“Our aim is to develop a model that will predict the 90-day mortality of different patients based on their gene profile, and so prevent the multiple-organ failure that leads to death.”
Running in tandem with Professor Evans’s research is the ADRENAL study, a project led by Wesley and Princess Alexandra Hospitals’ intensive care specialist, The George Institute for Global Health researchers and UQ professorial fellow Professor Bala Venkatesh, which focuses on hydrocortisone therapy.
The ADRENAL study is a multi-centre, randomised, blinded, placebo-controlled trial comparing intravenous hydrocortisone with placebo in critically ill patients with septic shock in intensive care. Around 3800 patients at 70 Intensive Care Units around the world are randomised to receive either intravenous hydrocortisone 200mg or placebo per day for seven days.
“The ADRENAL trial is the largest septic shock study to date. We are investigating whether the conflicting results of the two major corticosteroid trials were a result of the drug itself, or its reaction on different patients with a specific genetic make-up,” says Professor Venkatesh.
“It may be that corticosteroids would benefit some patients but could harm others, and the study led by Professor Evans could determine who will respond based on their genomic profile.”
Although more common in older adults and those with a weak immune system, sepsis and septic shock is becoming more prevalent and can happen to anyone. Hence the ongoing importance of discovering new treatments.
Sample collection for the genomic study will continue for the rest of 2017, with results expected in 2018. Results for the ADRENAL project are scheduled for publication at the end of 2017.
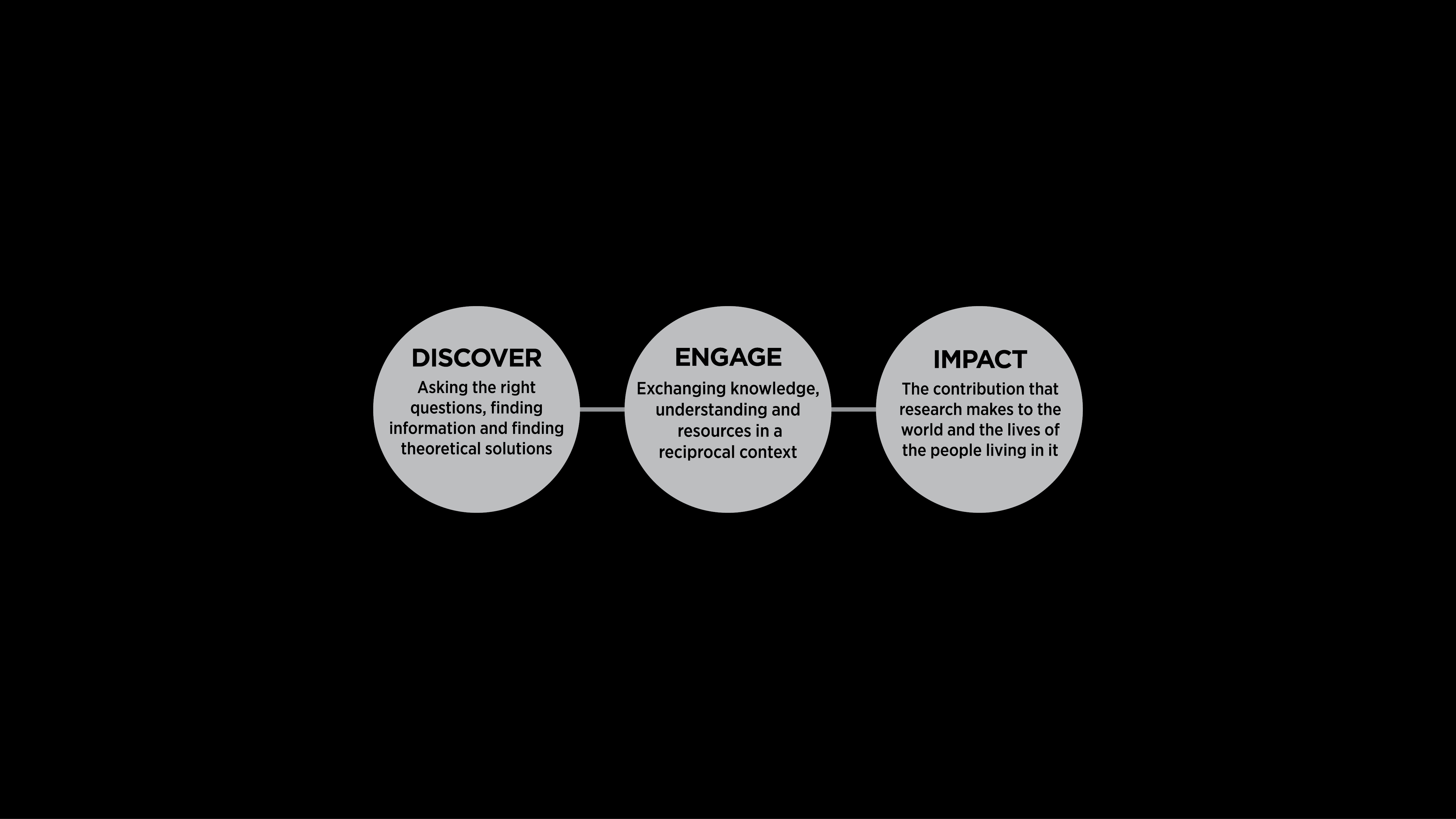
The story so far:
1997: Trials begin on alternative therapies for patients with severe sepsis
2003: French study (n=299) of low dose corticosteroids in septic shock shows suggestion of benefit
2008: European study (CORTICUS) (n=499) does not demonstrate any evidence of benefit with corticosteroids in septic shock. Results from these two studies generate considerable uncertainty among clinicians about the role of steroids and marked variability in practice: neither study has sufficient power to detect differences in mortality between steroids and placebo
2011: Professor Bala Venkatesh commences the ADRENAL (n=3800) study to determine if hydrocortisone, compared to placebo, reduces 90-day all-cause mortality in patients admitted to an ICU with septic shock
2011: Activated Protein C is withdrawn from market after trials failed to confirm its efficacy
2016: Professor David Evans collaborates with the ADRENAL investigators and establishes the ADRENAL Gene expression study – a genomic resource to investigate whether genetic variation between critically ill patients contributes to their susceptibility to bacterial infections, the severity of their disease and their response to treatment
2017: ADRENAL project results expected
2018: UQDI ADRENAL Gene expression study due to be completed
(Photo credit this page: iStock/Dr_Microbe_108268820, Opening page: iStock/Dr_Microbe_619963666; Rolling graphic: James North; Words by: Suzanne Parker)